Cancer Diagnosis
The prostate-specific antigen (PSA) has been widely used as a biomarker in current clinical practice to screen men for prostate cancer, although issues associated with this method including high false-positive rate are well known. This is because in addition to prostate cancer, infection and chronic inflammation or benign prostatic hyperplasia may also cause elevations in PSA levels. Therefore, there is tremendous interest in developing other approaches with higher specificity for improved detection of prostate cancer in recent years. Despite the significant progress in developing a number of new molecular biomarkers, none of them has been successful enough to replace PSA test so far. On the other hand, using exfoliated prostate cancer cells isolated from urine specimens for diagnosing the carcinoma of the prostate has long been proposed. Although the examination at cellular levels provides excellent specificities in contrast to PSA tests, past attempts at diagnosing prostate cancer via traditional urine cytology were abandoned due to unacceptably low sensitivities. The challenge in increasing sensitivity mainly stems from lacking sensitive and specific markers that allow visualization and differentiation of malignant prostate cancer cells through immunofluorescence labeling.
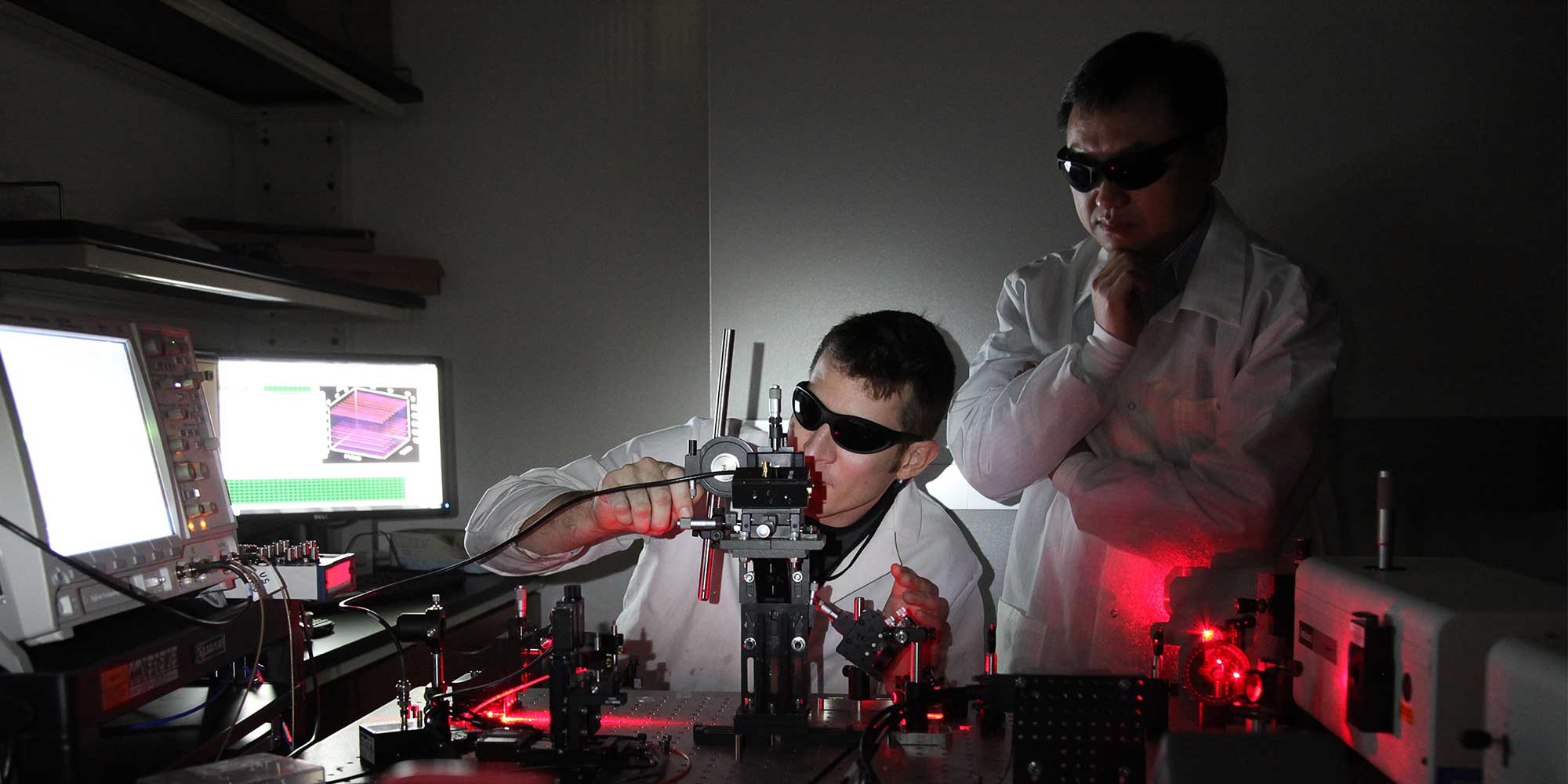
Instead of using immunofluorescence labeling, we have been working on a new approach utilizing a native contrast parameter of cells for label-free, noninvasive detection of prostate cancer. A novel imaging system based on a patented photonic crystal biosensor will be designed and constructed for label-free detection of malignant prostate cancer cells from urine with unparalleled sensitivity and specificity. Successful development of this technology will allow reducing unnecessary multicore prostate biopsy due to false-positive PSA results and address the unmet urgent demand of a noninvasive, accurate approach for prostate cancer screening.
New breast cancer treatments now include medications that target the overexpression of growth factor receptors, such as the proto-oncogene human epidermal growth factor receptor 2 (HER2/neu) and epidermal growth factor receptor (EGFR) to suppress the abnormal growth of cancerous cells and induce cancer regression. Although effective, certain treatments are toxic to vital organs, and demand assurance that the pursued receptor is present at the tumor before administration of the drug. This requires diagnostic tools to provide tumor molecular signatures, as well as locational information. In this study, photoacoustic imaging and fluorescence sensing by a fiber-optic probe have been utilized to characterize HER2 and EGFR overexpressed tumors in vivo. HER2 and EGFR antibodies were conjugated with ICG-Sulfo-OSu and Alexa Fluor 680, respectively, to tag BT474 (HER2+) and MDA-MB-468 (EGFR+) tumors. Mice with subcutaneous HER2+ and/or EGFR+ tumors received intravenous injections of the conjugates for photoacoustic imaging and fluorescence sensing. Photoacoustic images of the tumors were rendered with the novel weighted algorithm to view conjugate accumulation at the tumor sites. Fiber-optic fluorescence sensing was used to distinguish between tumor types through fluorescence intensity. This system offers a minimally invasive approach to characterize the molecular signatures of breast cancer in vivo.
Controlled Drug Delivery
Drug Toxicity Assays and Pharmaceutical Quality Control
Neuroengineering
We are grateful for the following funding agencies for their grant support of our research projects.
|
National Institutes of Health (NIH), including NCI, NIBIB, and NIGMS
|
United States Department of Defense (DoD)
|
|
National Science Foundation (NSF)
|
Cancer Prevention Research Institute of Texas (CPRIT)
|
|
United States Department of Agriculture (USDA)
|
San Antonio Area Foundation
|
|
San Antonio Life Sciences Institute
|
UTSA-SwRi Connect Grant
|
|
UTSA VPR Office
|
Harry S Moss Heart Trust |